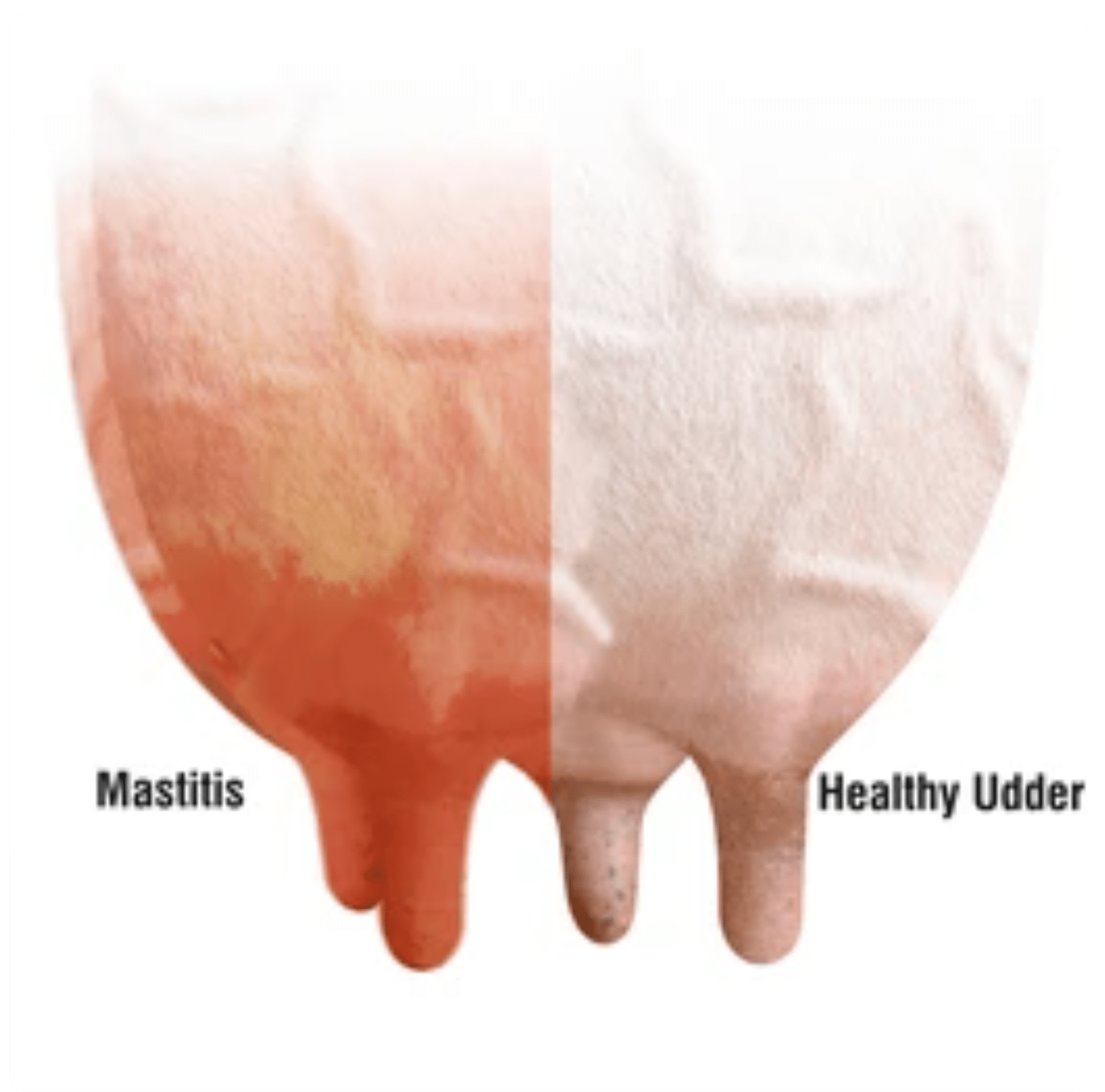
Bovine mastitis is a condition characterized by the persistent and inflammatory reaction of the mammary gland (udder tissue) due to either injury or infections caused by microorganisms. Matitis (Bovine mastitis) in dairy is very common and serious cattle disease. This condition not only reduces the amount of milk a cow produces but also affects the quality of the milk, sometimes making it unsafe for consumption. If not treated early, mastitis can lead to permanent udder damage and, in severe cases, even the death of the animal.
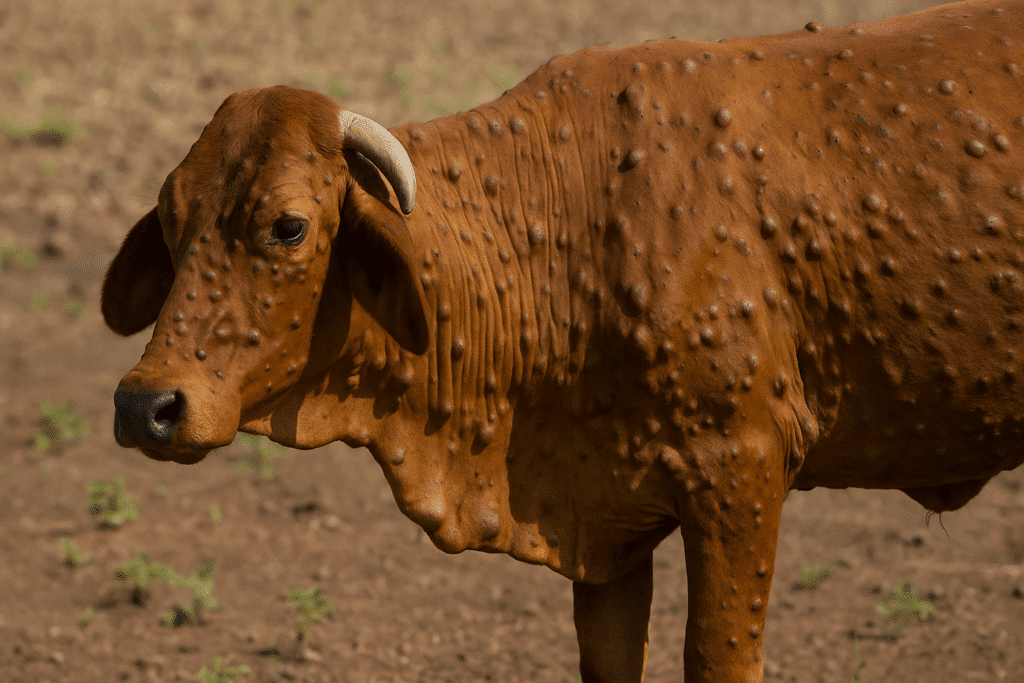
Mastitis is a painful inflammation of a cow’s udder, usually caused by bacterial infection, and it significantly affects milk production and quality. It leads to swelling, redness, and pain in the udder, while the milk may appear watery, clotted, or contain pus. Infected cows often show signs of discomfort, fever, or reduced appetite, and in severe cases, may lie down more often.
The disease can be clinical (visible symptoms), subclinical (no obvious signs but reduced milk and increased somatic cell count), or chronic (long-term and recurring). Mastitis in dairy cows is typically caused by bacteria such as E. coli or Staphylococcus aureus, often due to poor hygiene, dirty bedding, or milking equipment. Mastitis in cows treatment involves antibiotics and udder care, though severe cases may require culling. Preventing mastitis relies on good milking hygiene, clean environments, and regular udder health monitoring.
Mastitis Symptoms in Cows
Mastitis symptoms in cows can be recognized by inflammation of the udder, which becomes swollen, painful, and red. Signs of mastitis in cows can be identified by the presence of pus, blood clots, foul-smelling, watery, or light-colored milk, and a sharp drop in overall milk production. The infected area feels hot, and even a light touch can cause discomfort to the cow. Other signs of mastitis in cows include fever, loss of appetite, and difficulty walking due to the pain in the udder.
loss of appetite, and difficulty walking due to the pain in the udder.
In severe cases of mastitis, the infection can worsen, and cows may show more serious symptoms like sunken eyes, diarrhea, and extreme dehydration. A mastitis-infected cow may lose weight quickly and develop pus in the udder. Mastitis can lead to life-threatening conditions if not treated and identified on time. Early mastitis detection is possible with a simple California Mastitis Test (CMT), which checks for hidden (subclinical) infections before clear symptoms appear. Spotting mastitis early can save the cow’s health and help farmers avoid major losses in milk production.
Causes of Mastitis in Cows
Mastitis in cows is caused by outer infection or a wide range of microorganisms, including viruses, fungi, mycoplasma, and especially bacteria. Among these, bacterial infections are the most common culprits. The condition begins when microbes enter the udder through the teat canal, often following an injury or when hygiene is poor. Almost any microbe can take advantage of the opportunity to invade, but the most frequent offenders are species of Streptococcus, Staphylococcus, and gram-negative rods. Many of these are coliform bacteria—lactose-fermenting organisms typically found in the environment or the cow’s digestive system. Once inside, these pathogens multiply, leading to inflammation and discomfort. Good hygiene, proper milking techniques, and overall udder care are key to keeping mastitis at bay.
Treatment of mastitis in cows
Once mastitis is detected, basic first aid should begin right away. Applying ice cubes to the surface of the udder can help reduce swelling and pain. The infected milk from the affected teat should be carefully drained out three times a day and disposed of safely. To ensure hygienic disposal, a 5% phenol solution can be added to the infected milk before discarding it. During milking, it is very important to follow proper order—always milk the healthy, non-infected cows first, and milk the infected ones afterward to prevent the spread of infection within the herd.
Mastitis can be treated with intramammary antibiotics that go either directly into the udder  (intramammary) or into the whole body (systemic antibiotics), or sometimes both. If the mastitis is mild and only in one quarter, intramammary treatment usually works best. But if the infection is more serious or in more than one quarter, systemic treatment is better because it helps fight the infection throughout the cow’s body.
(intramammary) or into the whole body (systemic antibiotics), or sometimes both. If the mastitis is mild and only in one quarter, intramammary treatment usually works best. But if the infection is more serious or in more than one quarter, systemic treatment is better because it helps fight the infection throughout the cow’s body.
Intramammary Antibiotics for mastitis
To cure mastitis in cows Intramammary antibiotics are commonly used to treat mastitis in cows, as they are directly administered into the udder to target the infection at its source. These antibiotics work by killing or inhibiting the growth of the bacteria causing the infection, leading to improved udder health and better milk production.
Key Points about Intramammary Antibiotics:
- Application: The antibiotic is inserted directly into the affected teat through a special applicator or syringe. This ensures that the drug reaches the infection site quickly and effectively.
- When to Use: Intramammary antibiotics are typically used for mild to moderate cases of mastitis, especially when only one quarter of the udder is affected. They are most effective when the infection is localized.
- Common Antibiotics Used:
- Penicillin
- Cephalosporins
- Streptomycin
- Ceftiofur
- Dosage and Duration: The dosage and duration of treatment vary depending on the specific antibiotic used, the severity of the infection, and the manufacturer’s recommendations. Treatment usually lasts for a few days to a week.
- Withdrawal Period: After intramammary treatment, there is a withdrawal period, during which the milk from treated cows must not be used for human consumption. This ensures that any antibiotic residues are cleared from the cow’s system.
- Side Effects: In general, side effects are minimal if used correctly, but improper application can lead to issues such as teat injury or antibiotic resistance.
Systemic Antibiotics for Mastitis in Dairy Cows
What is Systemic Antibiotic Therapy?
Systemic antibiotics are medications administered via injection (intramuscular or intravenous) to circulate through the bloodstream and reach the mammary gland from within. This approach is often used when:
Mastitis is severe or acute, especially toxic mastitis
The infection may have spread beyond the udder
Intramammary treatment alone is not effective
Common Systemic Antibiotics Used in Mastitis
| Antibiotic Name | Route | Spectrum | Common Brands (varies by country) |
|---|---|---|---|
| Ceftiofur | IM/IV | Broad-spectrum (G+ & G-) | Excenel, Naxcel, Ceftiocyl |
| Oxytetracycline | IM/IV | Broad-spectrum | Terramycin, Alamycin |
| Penicillin/Streptomycin | IM | G+ (penicillin) + G- (strep) | Pen & Strep, Combi-Pen |
| Ampicillin | IM/IV | Broad-spectrum | Polyflex, Ampicare |
| Sulfadimidine-trimethoprim | IM | Broad-spectrum | Borgal, Tribrissen |
When is Systemic Antibiotic Use Indicated?
Severe clinical mastitis with systemic signs like:

Fever
Dehydration
Loss of appetite
Depression
Coliform mastitis (e.g. E. coli), which causes rapid toxin release
When infection fails to respond to intramammary antibiotics
For dry cow therapy in some severe or recurrent cases (systemic use at dry-off)
How They Work (Mechanism of Action)
Ceftiofur (3rd-gen cephalosporin): Inhibits bacterial cell wall synthesis; effective against both Gram-positive and Gram-negative organisms.
Oxytetracycline: Inhibits protein synthesis by binding to the 30S ribosomal subunit.
Penicillin/Streptomycin: Penicillin inhibits cell wall synthesis (G+), Streptomycin interferes with protein synthesis (G-).
Sulfadimidine-trimethoprim: Inhibits folic acid synthesis, affecting bacterial DNA replication.
Considerations and Precautions
Milk withholding periods must be observed to prevent antibiotic residues in milk.
Meat withdrawal times also apply.
Always follow veterinarian advice and label instructions.
Overuse or misuse can lead to antibiotic resistance.
Supportive therapy (fluids, NSAIDs like flunixin) is often necessary alongside antibiotics.
Culture and Sensitivity Testing
Before starting systemic antibiotics, it’s ideal to take a milk sample for bacterial culture and sensitivity testing to:
Identify the causative organism
Choose the most effective antibiotic
Avoid unnecessary or ineffective treatments
Sum up of Systemic Antibiotic
Systemic antibiotic therapy is a critical tool in managing moderate to severe mastitis, especially when local (intramammary) therapy alone is insufficient. Drugs like ceftiofur, oxytetracycline, and penicillin-streptomycin combinations are frequently used depending on the case and bacterial cause. Timely intervention, proper dosing, and supportive care greatly improve outcomes and animal welfare.
Importance of Proper Application:
For intramammary antibiotics to be effective, it is essential to follow proper milking hygiene and administration procedures. Ensure that the teats are clean before application and that the antibiotic is administered exactly as prescribed to avoid complications.
Intramammary treatment, combined with good herd management practices, can help control mastitis and improve milk quality.
Medicine for mastitis in cows
Medicine for mastitis in cows commonly includes penicillin, cephalosporins, ceftiofur, ampicillin, and oxytetracycline. However, the intramammary and systemic mastitis medicines are different. Intramammary antibiotics (administered directly into the udder) and systemic antibiotics (given through injection or orally) are used based on the severity of the infection. Intramammary antibiotics, such as penicillin, cephalosporins, and ceftiofur, are commonly used for localized infections in one or a few quarters. For more severe or widespread infections, systemic antibiotics like ceftiofur, ampicillin, and oxytetracycline are preferred, as they treat the infection throughout the cow’s body. These medicines target bacteria like Streptococcus, Staphylococcus, and E. coli, which are the main causes of mastitis.
Conclusion of Mastitis in Cows
In conclusion, bovine mastitis is a serious and common condition that significantly affects the health of dairy cattle and the quality and quantity of milk production. It is primarily caused by bacterial infections, which enter the udder through the teat canal, often due to poor hygiene, injury, or unsanitary conditions. Early detection and proper treatment are critical to prevent long-term damage to the udder and to avoid the spread of infection. Treatment typically involves the use of intramammary antibiotics for localized infections or systemic antibiotics for more widespread cases. Proper management, including good milking hygiene and careful monitoring of udder health, plays a key role in preventing and controlling mastitis. By addressing the condition promptly, farmers can ensure the health of their cows, maintain milk quality, and prevent economic losses in dairy production.
FAQs of Mastitis in Cows and Cattle
What causes mastitis in cows?
Mastitis in cows is caused by infection from microorganisms, including bacteria, viruses, fungi, and mycoplasma. However, bacterial infections are the most common cause. The bacteria typically enter the udder through the teat canal, often due to injury or poor hygiene. Common bacterial offenders include Streptococcus, Staphylococcus, and E. coli, especially coliform bacteria that are found in the environment or in the cow’s digestive system.
What is mastitis in cows?
Mastitis in cows is an inflammation of the udder caused by an infection, typically bacterial. This condition affects milk production and quality, leading to swelling, redness, and pain in the udder. The milk may appear watery, clotted, or contain pus, and infected cows often show symptoms like fever, loss of appetite, and discomfort.
How to cure mastitis in cows?
Mastitis in cows can be cured using intramammary antibiotics (applied directly to the udder) or systemic antibiotics (administered through injection or orally), depending on the severity. For mild cases, intramammary antibiotics like penicillin, cephalosporins, and ceftiofur are effective. For more severe or widespread infections, systemic antibiotics like ceftiofur, ampicillin, and oxytetracycline are preferred. Proper milk hygiene, draining infected milk, and using anti-inflammatory treatments are also important.
How to treat mastitis in cattle?
Treatment of mastitis in cattle involves antibiotics, either intramammary (directly into the udder) or systemic (via injection or orally), depending on the severity and the number of infected quarters. Intramammary antibiotics are used for localized infections, while systemic antibiotics are used for more severe or widespread infections. Early detection, proper milking hygiene, and managing the environment are essential in treating and preventing mastitis.
How to treat mastitis in dairy cows?
To treat mastitis in dairy cows, intramammary antibiotics are commonly used for localized infections, while systemic antibiotics are applied for more severe cases. Infected milk should be drained and disposed of safely. Applying ice cubes to reduce swelling and following proper milking protocols (milking healthy cows first) are also recommended. Good hygiene and early detection are key to preventing the spread of infection.
What causes mastitis in cattle?
Mastitis in cattle is caused primarily by bacterial infections, with common pathogens including Streptococcus, Staphylococcus, and E. coli. These bacteria often enter the udder through the teat canal due to poor hygiene, injury, or environmental contamination. Bacteria are the main cause, but viruses, fungi, and mycoplasma can also contribute.
What is mastitis in cattle?
Mastitis in cattle is an inflammation of the udder, usually caused by bacterial infection. It causes swelling, redness, and pain in the udder, while the milk may be abnormal in appearance. The condition affects both milk quality and quantity and can lead to severe complications if not treated promptly.